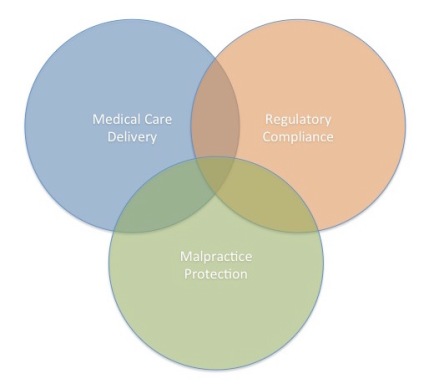
 Heath care documentation is done for three reasons.
Heath care documentation is done for three reasons.
1) Health care delivery (that’s the obvious one)
2) Regulatory compliance (checking all the boxes our government and payers think are important)
3) Malpractice avoidance (no one wants to get sued)
These three categories actually apply to every task we do in healthcare, but let’s confine this discussion to documentation.
Note in the accompanying figure, our three basic healthcare work requirements fit logically into a venn diagram. Much of what we do serves only one or two of the three driving purposes. In an ideal world, we work in the center of the diagram where all three converge. Unfortunately that “sweet spot” is pretty small, especially when it comes to documentation.
If all clinicians needed to do with our documentation was practice medicine (#1 above, blue in the attached Venn diagram), our notes would be more logical and much less bloated. Laundry lists of irrelevant and inaccurate diagnoses would not populate into every note. Copy and paste would occur a lot less often, and likely could be limited to appropriate uses such as carrying over past medical history (which should always be copy and pasted after verification to reduce errors). Only relevant physical exam findings would be reported, so these would not be lost in a sea of normals. Useful information that is not valued externally, such as personal touches – i.e. patient’s wedding anniversaries, achievements of their children, would have it’s own optimized workflow.
Regulatory compliance and malpractice protection, the #2 and #3 health care documentation purposes above, are responsible for the large majority of the drivel that shows up in our notes. Believe me, we doctors would all love to confine our work to health care delivery, but external forces box us into this uncomfortable place, and this creates junk documentation.
The result of trying to serve all of these missions results in the mess we have today. Healthcare IT expert Fred Trotter says that working with EHR is “like having a conversation with a habitual liar who has a speech impediment.”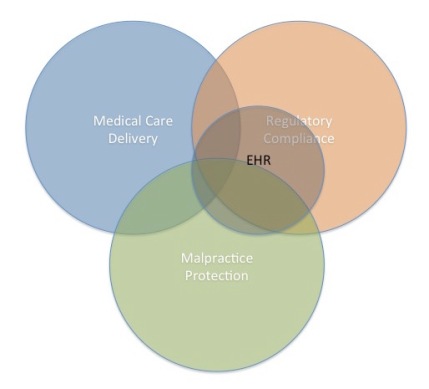
As I’ve diagrammed here, EHR serves all three basic functions, but not to equal degrees. EHR is designed for and sold to hospital administrators. Their first priority is business related – i.e. making sure the system runs efficiently and within the law. They work in the peach (Regulatory Compliance) circle. After the Federal Government stepped in with EHR incentives, Meaningful Use requirements created a set of requirements for the EHR companies that are about 90% peach-colored as well.
After satisfying the needs of administrators and the government, EHR vendors allot remaining resources to serving working clinicians seeing patients, as well as the patients themselves. This results in the lesser segment of EHR devoted to care delivery represented in blue.
Malpractice protection, the green circle, is a critical area of alignment for both the administrators and clinicians. EHR systems provide some degree of protection via completeness and automation, but also introduce new risks.
Since working clinicians don’t make purchasing decisions, what is an EHR vendor’s motivation to optimize the systems for care delivery? Note, also, that the enormous cost of each system coupled with a lack of easy data portability effectively locks in a healthcare system to their EHR. Nowadays, most physicians are employees of their hospitals and lack sufficient leverage to effect an expensive change, even if such a clinician-friendly EHR system were available.
EHR activities fundamentally service the task of Regulatory Compliance (the peach circle) as their primary mission. This satisfies both the hospital administrators and the government. Because all parties have limited resources, the contribution to the Health Care Delivery circle suffers. Both hospitals and clinicians are interested in Malpractice Protection, so the green circle is served at of mutual self interest, although EHR workflow only tangentially addresses this need.
Clinicians need mechanisms to streamline documentation so they can spend time with patients instead of in front of computer screens. Ironically, many of the efficiencies built into EHR to give clinician more time with their patients have become targets of disapproval for our regulators and critics. I find it frustrating when I hear pundits and government officials rally against copy/paste and templates (such as normal physical exam findings). Most of these critics have no perspective on running a busy clinic or inpatient service. It would be impossible to do our jobs without some degree of automation. Do you think the legal profession would consider eliminating templates and copy/paste? Do you think contracts and wills are written freehand each time? Ridiculous.
Good clinicians need to fight external forces to protect their ability to care for their patients. That means we need to devote the large bulk of our time and thoughts to working in the blue circle of healthcare delivery. That’s where our mission is served. The other two circles? We should click/copy/paste/dictate/template only what is necessary to prevent us from being sued, sanctioned, denied payment, or accused of poor quality. If we can do that efficiently, we can get back to taking care of our patients. One casualty of this appropriate triage is ugly documentation.
Folks need to stop confusing healthcare documentation with health care delivery. Those who grade and pay us give far too much weight to the former. Those actually taking care of patients know where to set their priorities.
Edward J. Schloss MD
@EJSMD
Adapted from my comments on EMR & EHR Forum post EHRs Don’t Make Errors, People Do.
Addendum 8/16/15: In response to a comment from Michael Katz MD @MGKatz036 discussing role of EHR in upcoding and other greed and fraud issues, I issued a lengthy comment/reply. Because it extends well my arguments above, I’ll include these as an addendum to the original post for better accessibility.
Mike, I’ve heard the concern that EHR causes fraud and increased cost charge many times. So much to say, but I’ll try to be brief
– E&M billing is already stacked against us. Leaving one irrelevant bullet point off the ROS list or physical exam can cause dramatic devaluation of an encounter. This is a playground for RAC audits and doctors live under that threat continuously. The system is illogical and need for attention to silly details draws up away from our primary mission. The EHR levels the playing field here. As I’ve said before, the dishonest MDs knew how to upcode dishonestly before EHR. Automation and reminders from EHR demystify the rules and lets honest doctors be fairly compensated. Do you have all the E&M rules memorized? Could your billing withstand an audit without the help of an EHR? If you were like many doctors, you’d just code level 3 and not take any chances. Ethical billing consultants (yes they exist) in the pre-EHR days found many doctors to be systematically undercoding because they didn’t want or know how to play the E&M game. If office charges go up after EHR, that may be entirely appropriate.
– How much free care is delivered now BECAUSE we have an EHR? I just spent 30 min on the phone doing two very complex patient evaluations involving EHR and remote pacemaker review. I did this at no charge. Without an EHR, this quality of care would be impossible without the paper chart. That means it won’t get done until tomorrow at the earliest, or I’d have to make do without the chart. In many cases we can prevent office and ER visits with this data access. Patient and system benefits, MD makes less money. It’s the right thing to do, so we do it.
– EHR charting is so painful, I often avoid the encounters altogether just so I don’t have to go through the misery of clicking through the documentation. The care gets delivered, I just don’t get paid. Lots of ways to do this, all ethical and appropriate. None violate our contracts. In the paper days, many of these would have been billed.
I decided not to include a circle on the venn diagram for unethical or inappropriate behavior. I have absolutely no doubt this exists and is a big problem. Nothing I say here denies this fact. This has been reported well and extensively by others.
Thanks,
Jay
@EJSMD
Excellent post… my only criticism is that this analysis is some what “corporate.” If you’ll allow me some cynicism…
I think you’re missing a large circle, which may or may not overlap with with Regulatory Compliance and Malpractice Protection (but not with Medical Care): Greed and Fraud.
Most doctors are good eggs and believe in several principals: document what you actually do and then bill for it. Overbilling (billing for stuff that isn’t done) is clearly fraud, but so is underbilling.
If you were to create a histogram of “appropriate” billing for doctors [not advanced practice providers], it should be a pretty normal distribution, with a median centering on Level 4. Some patients are hard (Level 5) and some are easy (Level 3), but most are average, right? (At least, I think that’s the definition of average.)
So, what happens if, by checking a few boxes, we find that our usual work can generate a Level 5 note, whereas in the past, we guessed that we would only bill a level 4?
[Herein lies the problem of perspective… procedural specialists breath a rarified air where Documentation pales on comparison to Surgery with regard to generation of income. As such, I’d say procedural specialists are in a special place, where there are limited incentives to Overbill. Rounding doctors and doctors with a primarily outpatient practice may have different incentives… potentially more in-line with actual purchasers of EMRs.]
There is a wink and a nod between EMR companies and their purchasers. The explicit promise: capture the work you’re actually doing.
We will be faced with a big moral / legal problem when 99% of Documentation is level 5.
The solution: Level 5 becomes the new average, and we invent Level 6 and Level 7 for the really hard patients.
Important point, Michael.
The corollary, though, is that the payers ALSO want all of that information in the EHR to allow for easy audit. Carrots and sticks.
The stick will be brutal when it strikes. If I were a payer, I would raise more than an eyebrow if pre-EMR X% of encounters were level 3-4 and post-EMR Y% were level 4-5.
Either the institution was previously underbilling (fraud) or is now overbilling (fraud).
…. all of these thoughts are predicated on the idea that EMRs change billing patterns. If they don’t, I would be interested to see those data.
I don’t usually believe the BS that appears in most automated notes which I get from corporate physicians, it is hard to believe that such a detailed robotic hx and obviously contrived px could be accomplished in a hurried 10 minute primary care visit. I often read these notes to the patient in point and they are often outraged by the blatant fabrications in the boiler plate. I find it frankly fraudulent and so do they.
Then… there are the “scribed” notes which are really silly.
I have been using an EMR of my own design since 1983 and we are constantly evolving it. I don’t give a rip about what the government calls “meaningful use”…. my version is true meaningful use and it’s a lot more efficient to use a program written by a clinician. I may not be getting the Obamacare kickbacks for my EMR but my system’s efficiency allows me to practice good medicine and spend quality time with my patients.
Mike, I’ve heard the EHR causes fraud and increased cost charge many times. So much to say, but I’ll try to be brief
– E&M billing is already stacked against us. Leaving one irrelevant bullet point off the ROS list or physical exam can cause dramatic devaluation of an encounter. This is a playground for RAC audits and doctors live under that threat continuously. The system is illogical and need for attention to silly details draws up away from our primary mission. The EHR levels the playing field here. As I’ve said before, the dishonest MDs knew how to upcode dishonestly before EHR. Automation and reminders from EHR demystify the rules and lets honest doctors be fairly compensated. Do you have all the E&M rules memorized? Could your billing withstand an audit without the help of an EHR? If you were like many doctors, you’d just code level 3 and not take any chances. Ethical billing consultants (yes they exist) in the pre-EHR days found many doctors to be systematically undercoding because they didn’t want or know how to play the E&M game. If office charges go up after EHR, that may be entirely appropriate.
– How much free care is delivered now BECAUSE we have an EHR? I just spent 30 min on the phone doing two very complex patient evaluations involving EHR and remote pacemaker review. I did this at no charge. Without an EHR, this quality of care would be impossible without the paper chart. That means it won’t get done until tomorrow at the earliest, or I’d have to make do without the chart. In many cases we can prevent office and ER visits with this data access. Patient and system benefits, MD makes less money. It’s the right thing to do, so we do it.
– EHR charting is so painful, I often avoid the encounters altogether just so I don’t have to go through the misery of clicking through the documentation. The care gets delivered, I just don’t get paid. Lots of ways to do this, all ethical and appropriate. None violate our contracts. In the paper days, many of these would have been billed.
I decided not to include a circle on the venn diagram for unethical or inappropriate behavior. I have absolutely no doubt this exists and is a big problem. Nothing I say here denies this fact. This has been reported well and extensively by others.
Thanks,
Jay
@EJSMD
I endorse everything you wrote above. 🙂
Sidenote: what do you think of the following inpatient follow-up note? (I stole this from Happy Hospitalist blog. It’s really good. Worth reading carefully.)
S) No new problems
O) 120/80 80 Tm 98.6
PE Alert, anxious, regular rhythm, normal femoral pulses, lungs clear, normal respiratory effort, bowel tones present, no tenderness, no clubbing, no synovitis, no rash
Labs INR 1.7 on Coumadin
CXR film personally reviewed-normal .
Discussed antibiotic options with Dr Smith,
A) Nothing needed
P) Nothing needed.
Would you believe that it satisfies the highest possible level of billing?
– physical exam: 3 vitals is 1 organ, 6 areas, 12 bullets
– high risk for drug management requiring intensive monitoring for toxicity
– (2 points-Data for discussion of case with another healthcare provider).
This being said, how would you compare the readability to the average Epic note? Much better, right?
That’s because it’s a lot easier to believe that a long ass Epic note is a Level 3 follow-up, rather than a highly readable progress note.
In a perfect world, Watson-esque AI would just look at the note and figure this out rather than forcing you to click a bunch of boxes to create a long note that says nothing.
Ah. That note is a blast from the past. So beautiful. Please repost in bad handwriting. Brings back some solid memories from the good old days.
Several other problems with EMR/EHR’s:
1) ‘Copy & Paste’ is possible WITHOUT an Audit Trail, such as:
elements of this note were copied by Dr. Note Writer on Today’s date from a note dated: Several days ago, written by
Dr. previous note writer and pasted into Today’s Note on Today’s Date. Without such an ‘Audit Trail,’ most EMR’s/EHR’s
could be considered to permit (or promote) plagarism, perpetuate errors from Copied Note, and possible moral and ethical
issues (? ‘mis-statements’).
2) A commentary in ACP Hospitalist recommended AGAINST writing in the active voice (as suggested strongly by
“Strunk and White.” Writing, for example, “The skin was cleansed and sterilized with Clorhexidine” doesn’t mention
who did this, omitting the operator’s name( same with “The skin was incised using cautery, scapel, with control of
bleeding with cautery and small hemostats.” Again, who did this procedure?
3) Back (not so long ago) Physician, Nurses, Respiratory, and other bedside providers all wrote in the progress note sections
of the patient chart-Ideally dated and timed. Now, using Cerner and Epic, I can’t sometimes find the Pre-Op or Post-Op notes,
Respiratory Therapy notes, etc. At times, in pre-Op, IntraOp Nursing, and post-Op notes, all I can find is something like this:
“The patient’s gender, ethnic, personal, and psychological needs were all addressed.” Where was the cautery ground? How were
the patient’s limbs placed/restrained? Even still, many Anesthesia flow sheets and notes remain hand written-there isn’t
a download of monitoring parameters-Amazing how few Oxygen desaturationsl, hypotensive, or hypertensive episodes
are found!
3) Patient records are frequently stored in servers off site(not in the local Medical Center Server-Cerner uses servers in
Kansas City, MO, their corporate Headquarters… What happens when these servers fail, even transiently? OMG, how can
physicians, etc. provide acceptable care when the EMR/EHR records are unavailable? There are frequently No Backups
and no ‘FailSafe’ protocols exist…